“I didn’t realise he could die.” How a mother is navigating the life-threatening challenges of a child with 11 severe allergies

Not long before her son’s first birthday, Katie Jennings refused to leave her GP surgery unless they prescribed him an EpiPen. Two weeks later it saved his life.
By Jules Millward
Yann’s first allergic reaction was at his eight-week immunisations. By seven months old, he had been diagnosed with an egg, peanut, and milk allergy.
As he was exposed to more foods, his reactions became increasingly more life-threatening.
It was only after seeing a campaign on Facebook that Katie, who lives in Cardiff, realised the severity of Yann’s allergies.
Katie said: “I didn’t realise he could die.”
Her doctor initially told her that he wouldn’t need the EpiPen, but she insisted he be given the essential medication.
She added: “As it became obvious that I wasn’t going to leave the room until I had a prescription, she reluctantly gave me one on the basis that I was having it as a six-month trial.
“Within two weeks, I had to use it.”
Yann reacts instantly if he comes into contact with an allergen. Photo: Katie Jennings
Yann reacts instantly if he comes into contact with an allergen. Photo: Katie Jennings
Latest research from Imperial College London estimates that the number of people living with food allergies in England has increased significantly between 2008 and 2018.
The analysis published in the journal Lancet Public Health found that up to 4% of preschool-aged children have a food allergy. In adults, this was one per cent, with these figures thought to be representative of the UK.
Imperial College London found those with a previous severe reaction weren't offered an EpiPen. Imperial College London via X
It also reported that many people who had previously had a severe reaction from a food allergy were not prescribed the lifesaving treatment.
Katie said that at no point had she been offered an EpiPen until the day she demanded one be prescribed.
The only information she had been given was a leaflet and told to remove all nuts from her house.
She added: “They were not offered at all by the hospital, and they’re still not offered, even when the children have blood tests which show that they’re very likely to go into anaphylactic shock.”
Yann has to take daily medication to stay safe. His allergies include severe eczema, asthma and hay fever. Photo: Jules Millward
Yann has to take daily medication to stay safe. His allergies include severe eczema, asthma and hay fever. Photo: Jules Millward
The doctor's reluctance to prescribe the EpiPen, along with the fear of an allergic reaction, wasn’t the only thing Katie had to worry about when coming to terms with Yann’s allergies.
Research from the University of East Anglia shows that 42% of parents of children with allergies meet the clinical threshold for post-traumatic stress symptoms.
The study also found that 39% of these reported moderate to extremely severe anxiety and that parents whose child had to have an EpiPen administered were seven times more likely to experience PTSS.
Katie was unable to do the things a new parent would usually do such as go to mother and baby groups or soft play due to the risk of contamination.
She said: “How on earth do you manage something that extreme, across that many food groups when you have a toddler that is crawling around putting food in their mouth?”
She also experienced a huge lack of awareness and understanding from people around her and felt unsupported and isolated.
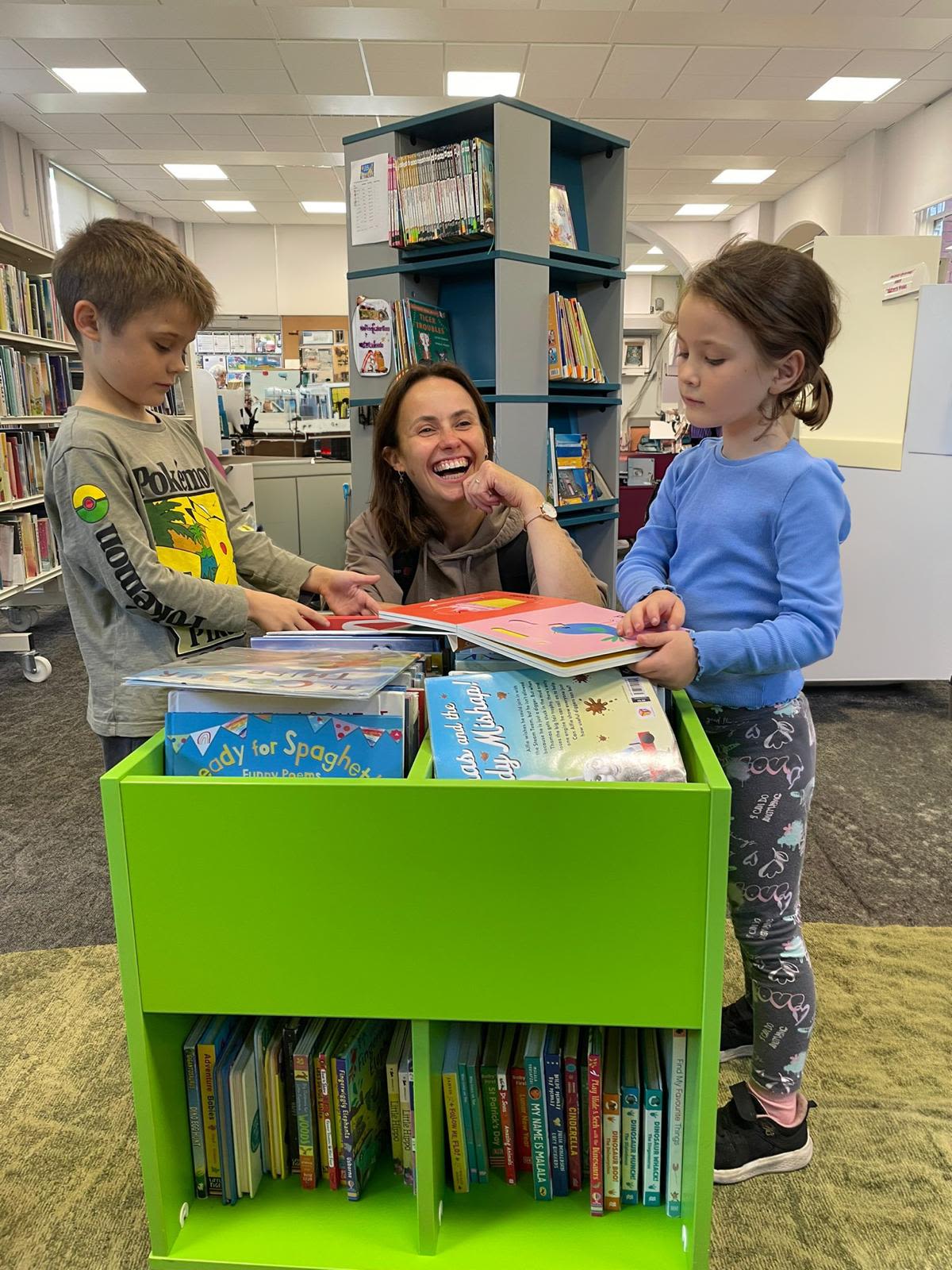
Katie often found herself doing things alone with Yann. The severity of his allergies meant many baby groups were not safe for them. Photo: Jules Millward
Katie often found herself doing things alone with Yann. The severity of his allergies meant many baby groups were not safe for them. Photo: Jules Millward
She added that it was “just too much” as she was on her own a lot.
“It was horrible for a long time.
“I struggled with it more, because of a lack of understanding…people just generally don’t get it.”
Katie didn’t want Yann to miss out, so she made it her mission to educate herself and others around her, to give him a childhood with as little restriction as possible.
Katie tries to keep Yann's life as normal as possible. His little sister Mai also has allergies, although not as severe. Photo: Jules Millward
Katie tries to keep Yann's life as normal as possible. His little sister Mai also has allergies, although not as severe. Photo: Jules Millward
Katie spent hours every week researching treatments and ways to keep Yann safe.
She joined Facebook groups which gave her a community of millions of parents around the world. These families could share their experiences, and support each other, even if it was from afar.
Through these groups, Katie found a way for Yann to attend school safely. Something she didn’t think would be possible with the severity of Yann's allergies.
With up to 17% of fatal anaphylaxis reactions in school-aged children happening while they are at school, knowing how to use an EpiPen is vital in an educational setting.
Whilst Anaphylaxis UK used to provide this training for free, the charity now charges for the life-saving course, making it inaccessible to many schools.
This means it often falls on the parents to educate the school on what to do in the case of anaphylactic shock.
Anaphylaxis UK offer training for schools, but have recently started charging for it. Anaphylaxis UK via Instagram
Katie worked with the school for two years before Yann was due to make it safe for him to attend.
Every year she meets with his new class teacher to train them in how to use an EpiPen, along with helping to put safeguarding procedures in place.
The school had dealt with children with life-threatening allergies before, but they had never had a student as complex as Yann.
Although it falls on Katie to coordinate with them, she expressed how receptive and accommodating they have been.
She said: “We got very lucky with our school. They are so open-minded, and they are all about inclusion.”
Katie added: “If that school could be used as a blueprint for how to manage kids with allergies, that would save so many lives and I think would prevent so much stress in parents.”
Ella Lewis is a teacher in the school and worked closely with Katie when Yann was in year two. She coordinated a class Christmas party that was safe enough for Yann to attend, the first one he was able to be a part of.
Miss Lewis said: “Yann had the best time…he just felt comfortable, he felt safe, and the children were brilliant.”
She added that there are key things other schools can put in place to help accommodate children with severe allergies.
“They can make sure they have those relationships with parents and that they have the knowledge and understanding to be able to create those safe environments.”
The fight for adequate allergy training is not just limited to schools. There is also a huge lack of awareness in the food industry.
This has been highlighted by the tragic death of Hannah Cook, a schoolgirl who died after taking a sip of a hot chocolate from Costa Coffee. It was made with cow’s milk instead of soya milk, even after her mum had made them aware of her allergy.
The 13-year-old did not have an EpiPen on her, and after being rushed to a local pharmacy who were able to administer medication, it sadly was not enough to combat the effects of anaphylactic shock.
Deaths like this could be avoided, and while there have been changes, there is still much that needs to be done.
The Natasha Foundation was set up by the parents of Natasha Edan-Laperouse, who died after eating a baguette from Pret a Manger.
At the time, a loophole in the law meant pre-packaged food made and sold on the same premises didn’t have to list their ingredients, meaning they were unaware it contained sesame, an ingredient she was highly allergic to.
The foundation fought for change and in 2021, Natasha’s Law was implemented. This law requires food outlets to provide a full list of ingredients with clear allergen labelling on their pre-packaged for direct sale foods.
They are now campaigning for the government to appoint an Allergy Tsar, who would act as a public champion for those with allergies.
The Natasha Foundation are campaigning for an Allergy Tsar to be appointed whose job would be to advocate for people with allergies. The Natasha Foundation via Instagram
Incidents like these make it difficult for a child with allergies as severe as Yann’s to live a life without fear and it is unlikely he will be able to attend high school safely.
With her determination to keep his life as normal as possible, Katie shows a strength and resilience like no other and continues to advocate for him every day.
"Doing nothing is essentially accepting a death sentence for Yann"

Since Yann’s diagnosis, his parents have had to plan, prepare, fight and organise every single day to give him the same opportunities as his peers.
As he gets older and becomes more independent, it will be harder for them to protect him from the allergens that could kill him.
Yann is not eligible for the advanced treatments offered in the UK due to the severity of his allergies.
But there is hope for the future. The Jennings have recently travelled to America to start a life-changing treatment with The Food Allergy Institute in California.
The Tolerance Induction Programme helps children & young adults overcome their severe food allergies.
With a 99% success rate, this ground-breaking treatment could put Yann into complete remission, giving him the chance at a normal life.
Dr Inderpal Randhawa discussing the Food Allergy Institute's groundbreaking milk study, which had a 100% remission rate. Food.allergy.institute via Instagram
The treatment will cost the family over £100,000. They have raised enough money for the first stage of the treatment, but their fundraising efforts will be ongoing until he completes the programme.
It is a small price to pay for the chance of Yann living without the threat of fatal anaphylaxis every single day.
This treatment was available to Yann two years ago, but because of the danger flying posed, they were unable to go.
Katie didn't give up, and after extensive research found reassurance and safety in British Airways allergy policy. This made it possible for them to travel to California for the first stage of the treatment.
They were able to board early and wipe down the seats for any traces of nut dust, and announcements were made throughout the flight asking passengers to refrain from eating nuts during the flights.
Katie said: “BA’s policy and attitude in accommodating people with allergies should be promoted and celebrated.”
With Love Island star Jack Fowler recently suffering from anaphylactic shock on an Emirates flight, this proactive approach to accommodating passengers with severe allergies will come as welcome news to those who have been unable to travel in the past.
Yann and his parents will have to travel to the clinic in LA every 12 weeks for in-person clinical sessions, for a minimum of five years.
Their home, work, and school life will be impacted. The whole family will have to isolate for a week before each trip.
Katie said: “Doing nothing is essentially accepting a death sentence for Yann, and when a treatment that works exists, we have to make it happen.”
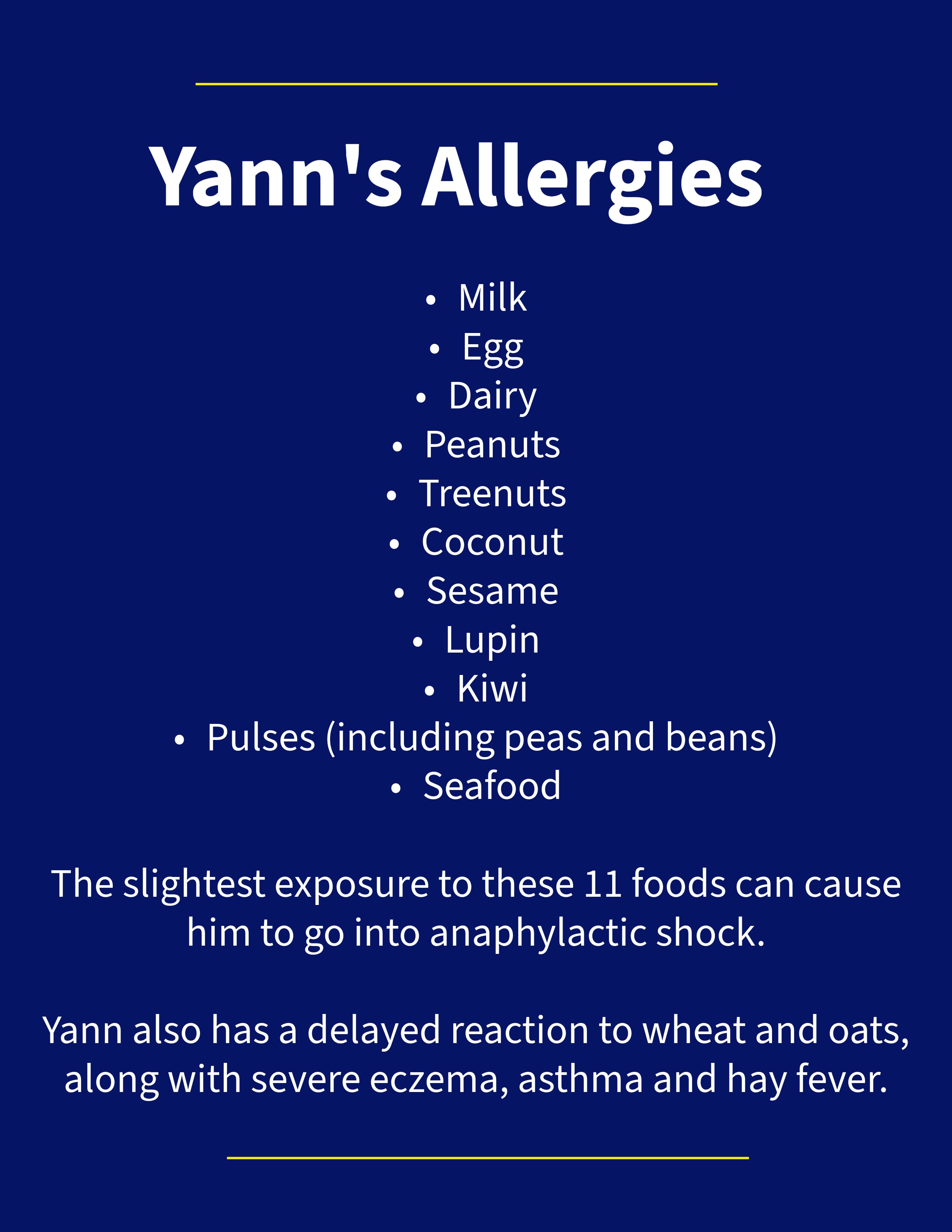
Yann is allergic to 11 foods, some of which are often used as an alternative in free from foods, making it harder to avoid. Graphic: Jules Millward
Yann is allergic to 11 foods, some of which are often used as an alternative in free from foods, making it harder to avoid. Graphic: Jules Millward
She added: “After this, he will have as good a chance as anyone else of living and enjoying a full and healthy life.
“He will be able to live without all the ridiculous restrictions and safety nets that we have to navigate. Suddenly, things that are currently off limits will open as options to him.
“This is going to change everything for the better.”
*You can donate to Yann's fundraising page here
"We are recognising things better."

Allergies have now been recognised as a global health issue by The World Health Organisation, with figures from Allergy UK showing allergies cost the NHS over £1 billion a year.
Dr Sherif Khalifa is a GP who specialised in paediatrics. He worked in the children’s allergy clinic in Cardiff for two years where he developed an expertise in paediatric allergies.
Dr Khalifa said that the rise in allergies is partly due to increased recognition and awareness.
He said: “I think we are recognising things better in our children. I think we as doctors are recognising as well, the parents are telling us that, so we are acting upon that.”
Dr Khalifa explained that the traditional approach to allergies has usually been avoidance and treatment of reactions.
Patients should cut out that food group entirely, and avoid contact but that it is “not 100 per cent effective.”
To treat the allergy, they would be given medication.
He added: “If a child accidentally came into contact [with some eggs or peanut butter for example] you’d give them antihistamines, you’d give them steroids if needed, or an EpiPen.
“But now we’re moving on to immunotherapy, which is ways of training the immune system to get used to allergens.”
Palforzia is an immunotherapy treatment that has recently become available on the NHS in England. Palforzia_RX via Instagram
Palforzia is an immunotherapy treatment that exposes a child to minuscule amounts of peanut in a controlled environment.
The initial phase is a minimum of 22 weeks, with the dose being built up fortnightly, then a maintenance dose for 6-18 months. The aim is for patients to build up to safely being able to consume a small amount of peanut every day.
Dr Khalifa said: “There is a small risk of anaphylaxis with Palforzia and all other allergies need to be well controlled before prescribing it.”
It is thought that patients could lose tolerance if the treatment stops, but with one in 50 children in the UK having a peanut allergy, this treatment could be life-changing for those who are eligible.
It is available in England and has recently been approved in Wales. Dr Khalifa thinks this is a positive step.
He said: “It is a really cost-effective treatment, it’s great for the NHS.”